It is a bright Tuesday morning, and the soft and diffuse sun rays are piercing through Ringa-Kojwach village in Homa Bay County, in south western Kenya.
Cynthia (not her real name), clutching her one-year-old baby, is making her way into this must-attend meeting at a neighbour’s compound.
She is on time, just like her 19 other colleagues.
Attendees of the meeting are members of Upendo Support Group, bringing together 20 women living with HIV, and fighting to prevent transmission of the virus to their unborn and breastfeeding babies.
Twenty-five year old Cynthia discovered her HIV status in 2020 while three months pregnant with her second born child.
“I had been feeling sick for some time but never sought treatment. So this day I was overwhelmed and I was taken to hospital. It was then that I discovered that I was three months pregnant and HIV positive. I was devastated,” she said.
Cynthia was enrolled for HIV treatment and antenatal care, but this was too late to save her baby who was born with the virus.
“This was a new journey in my life. Having to care for myself and my baby,” she said.
HIV Support groups
But all was not lost. It was during her post-natal care that she was linked to this support group to help manage her condition and that of the baby.
“Through these sessions, I managed to shed off the stigma, get back to my feet, accept the situation and focus on care and treatment for myself and my baby,” she added.
And it was here that she got the confidence to conceive again, against her own fears and societal pressure that it was not advisable for her to continue bearing children.
She conceived, and this time round, she adhered to the HIV treatment and care, delivering her third born baby who is free from the virus, and has near zero chances of contracting it.
Cynthia’s story is shared by 29 year old Jane (not her real name) who is also a member of this group.
In 2012, Jane got her first born baby. Three months into lactation, her health began to deteriorate followed by wounds all over her body. Examinations at the hospital revealed that she was HIV positive. She was immediately enrolled for HIV care and management.
Subsequent HIV tests however revealed that the baby had contracted the virus.
“I had attended a few pre-natal visits, and I had tested negative for the virus. I however delivered at a traditional birth attendant’s, and I did not take the baby to any medical facility until the day I went to hospital for my illness,” she said.
“I had wounds in my entire body, including my breast, and I guess that is how my baby contracted the virus when breastfeeding,” she added.
Jane, just like Cynthia was scared and depressed. She contemplated suicide and killing her baby. She however got help from her peers at the hospital, regained hope and swore never to give birth again.
It was during her troubled life that she joined Upendo Support Group and began her journey of emotional recovery. Last year she delivered her second born baby, free from the virus.

Ending mother to child transmission
The UNAIDS standards for HIV epidemic control (UNAIDS 95-95-95 targets) requires that 95 per cent of all people living with HIV (PLHIV) are diagnosed, 95 per cent of all PLHIV are on treatment and 95 per cent of all PLHIV are virally suppressed.
The current UNAIDS 95-95-95 progress among adults is 95-95-90. However, among children the performance is 85-85-74.
In September 2023, Kenya launched an action plan dubbed ‘Kenya Plan to End AIDS in Children by 2027’. The strategy aimed at ending new HIV infections among children through mother to child transmission.
During the launch of the program on September 8, 2023 in Homa Bay County, Health Cabinet Secretary Susan Nakhumicha noted that through collaborations and partnerships over the last ten years, Kenya reduced new HIV infections by 57 per cent, and AIDS-related death decreased by 68 per cent.
“However, mother-to-child transmission rate remains high at 8.6 per cent, treatment coverage children living with HIV is 85 per cent with about 74 per cent of those virally suppressed. This is concerning as children have been left behind and their voices remain unheard,” she said.
According to Justus Ochola, head of Research, Innovation and New Learning unit within the Department of Health in Homa Bay County, Upendo Support Group is taking the lead as one of the local interventions that is working towards achieving zero mother to child transmission.
Table banking to fight HIV
Upendo Group’s Coordinator, Lucy Atela, says the entity was formed following mother to child transmission scares which had hit the county.
“In 2008, ten of us began the journey. Adherence to HIV treatment was the biggest concern due to high levels of stigma. We needed to unite to face our fears,” she says.
A decade later, the attitude has changed, and Ms Atela says members of the group have borne 12 babies since 2018, and guess what! All of them are free from the virus.
Members have realised that their table banking is not similar to the common ones out there. It is an initiative to save our children from HIV. This is the push behind the commitment to make this project work
Upendo Group’s Coordinator, Lucy Atela
The feat, Ms Atela says has been achieved through various initiatives including a robust table banking program.
The program sees the women save at least Sh300 (USD 25) every Tuesday when they meet. Members then borrow the money to engage in various economic activities for economic stability.
“We discovered that apart from stigma, the other major contributor to HIV adherence challenges was hunger,” said Atela.
Ms Atela says some members of the group would skip drugs due to lack of food.
“HIV medication are strong and you cannot take them in an empty stomach, so some people would avoid the medication all together, and this would mean a hike in viral load which would be passed to the unborn or breastfeeding babies,” she said.
The table banking venture was therefore a saving grace for economic empowerment to enable the members have income generating activities which in turn facilitated group members purchase balanced diet.
Cynthia and Jane have been taking loans from the group. Cynthia used her loan to start a fish selling business with subsequent top ups contributing immensely to the business and other domestic needs.
Jane utilises her loan to buy household goods in wholesale, and hawks them in nearby markets and homes.
“Once in awhile I use the profit to pay school fees for my child in school. I also never lack what to eat,” she says.
Ms Atela says the group has never faced challenges of loan defaulting.
“Members have realised that their table banking is not similar to the common ones out there. It is an initiative to save our children from HIV. This is the push behind the commitment to make this project work,” she noted during our interview held at a media science café organised by the Media for Environment, Science, Health and Agriculture (MESHA).
The group has also been working with local health facilities in reducing mother to child transmission of HIV through peer education, follow ups on treatment, and information sharing on HIV testing and care.

According to the National Syndemic Disease Control Council, Homa Bay County had HIV prevalence of 15.2 per cent in 2023, down from over 23 per cent a decade before.
Ochola observes that a lot has gone into achieving this fete, especially on mother to child transmission.
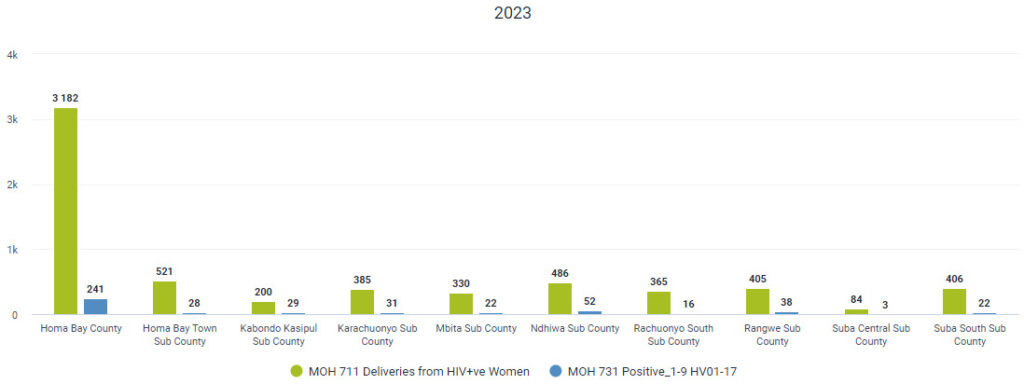
According to records from the County Health Department, the county recorded 3, 423 deliveries by HIV positive mothers.
Out of this, only 241 babies were born HIV positive.
“This translates to about 5.3 per cent mother to child transmission, down from 18 per cent in 2012,” said Ochola.
According to Mr Ochola, innovative interventions such as enhanced HIV testing within the communities, and robust follow up to ensure adherence to treatment have greatly contributed to the reduced cases of infections.
“When a pregnant mother is on treatment and the viral load become undetectable, the chances of transmitting the virus to their babies is almost zero,” said Ochola.
In 2023, Mr Ochola notes that 20, 345 pregnant women were tested for HIV. This represented 99 per cent of pregnant women during the period. The test is aimed at ensuring that all pregnant women know their HIV status as the first line of curbing mother to child transmission.
“As we speak, 99 per cent of all pregnant women know their HIV status, and about 94 per cent of the entire Homa Bay County population have been tested in the last one year,” he added.
Out of 100 deliveries in the county, Mr Ochola says about 78 take place within the hospitals, up from 48 in 2012.
“Our objective is to have every pregnant woman deliver in hospital and start antenatal clinics in good time so that we drive the country to achieving the elimination of mother to child transmission,” he added.
Additional reporting by Kevine Omollo
