Post-Partum Haemorrhage (PPH) is among the leading causes of maternal mortality in Kenya, contributing to 34% of maternal deaths.
World Health Organisation (WHO) defines PPH as losing more than 500 millilitres (ml) of blood 24 hours after vaginal birth, and more than 100 ml of blood after a caesarean (C-section) birth.
Similarly, PPH can also be defined as excessive bleeding and loss of blood occurring shortly after giving birth.
The condition is commonly caused by the uterus not contracting properly after birth.
Migori County is among the 15 counties in Kenya grappling with the issue of maternal deaths, with PPH among the leading direct cause of these deaths.
However, the condition is treatable only if a woman delivers at a health facility that has the right tools.

During the birth of my third child, I lost a lot of blood until I could not feel myself. I was completely unconscious, I thought I was going to die
Millicent Akoth
Millicent Akoth is a young mother of three in the rural Kameji location in Migori County.
She shares her ordeal with PPH.
“My previous deliveries were successful. I did not lose a lot of blood after delivery. However, the delivery of my last born came with a lot of problems,” she narrates
Complicated delivery
Millicent recounts how the problem started when her third child came earlier than usual.
Her delivery came in the seventh month.
The birth was accompanied by excessive bleeding and much loss of blood, sending her unconscious.

“During the birth of my third child, I lost a lot of blood until I could not feel myself. I was completely unconscious, I thought I was going to die” she continued.
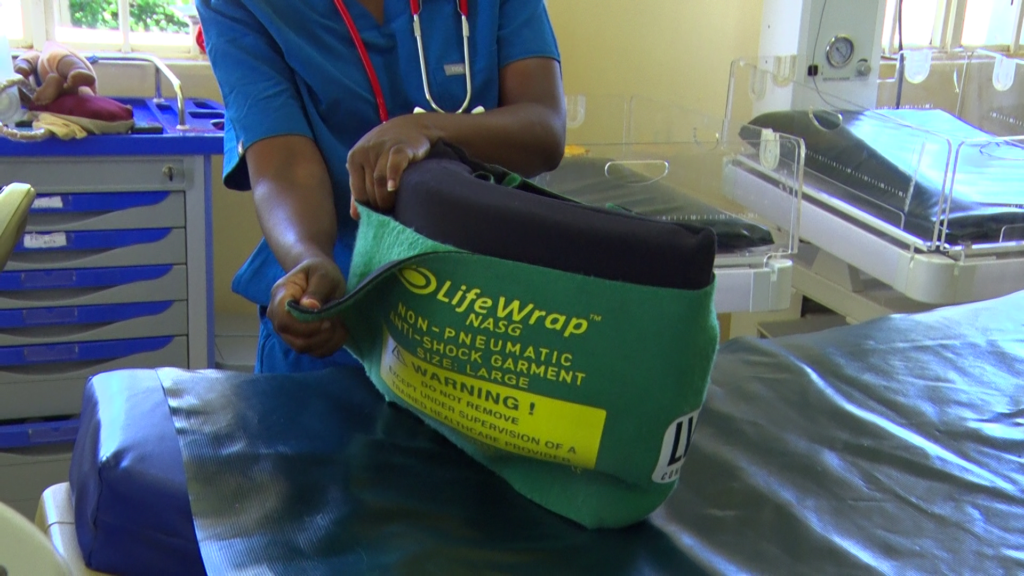
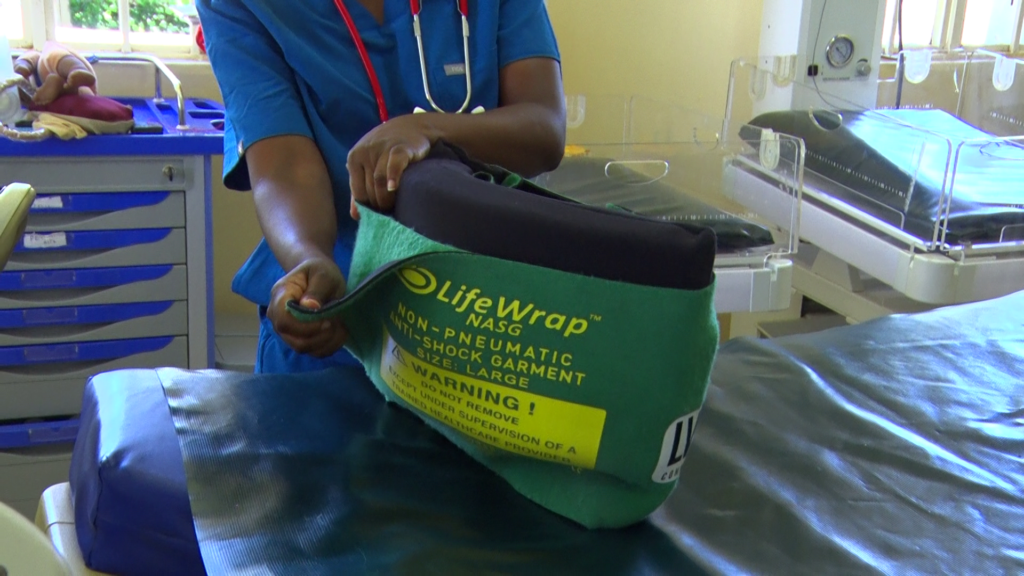
In Millicent’s case, it was a quick intervention by medical staff at the health facility, who put her under the Non-pneumatic Anti-Shock Garment (NASG).
However, she narrates that should she have delivered at home, maybe she could have lost her life or the baby’s.
“I was put inside a green garment strap from my legs upward to my abdomen. It was then that I regain my consciousness,” says Millicent.
Double trouble
In 2021, Jane Akinyi, a resident of Nyatike sub-county was rushed to a local health facility by her brother after experiencing excessive bleeding during childbirth.
The birth came unannounced.
“We had just concluded having breakfast when I felt the rapture. I was home alone with my brother who knew nothing about delivery and this led to more bleeding. The hospital was also a distance from home,” narrates Jane.
The journey to the hospital was a daunting one, as the poor state of the roads in the area made it difficult for ambulances to navigate.
Jane feared that the delay caused by the bumpy and treacherous journey would have dire consequences for her health.
Upon arriving at the hospital, Jane was quickly attended to by a team of doctors and nurses.
She was diagnosed with postpartum haemorrhage (PPH) and referred to Migori County referral hospital for urgent medical attention.
Timely intervention
Her condition was severe, and the medical team decided to use a Non-Pneumatic Anti-Shock Garment (NASG) to stabilize her.
The timely intervention of the medical team and the use of the NASG ensured Jane’s condition stabilized within a few hours.
“I believe that garment they wrapped around me played a critical role in stabilizing my condition and saving my life
Jane Akinyi
A few days later she was discharged and went on to make a full recovery.
“I believe that garment they wrapped around me played a critical role in stabilizing my condition and saving my life,” she recounts.
The Non-pneumatic Anti-Shock Garment (NASG)

NASG is a fit-for-purpose emergency garment, that has been proven to save women’s lives by reducing blood loss and stabilizing the patient until treatment is available.
As a mechanical device, it offers compressions on the blood vessels.
The garment is divided into six parts called segments.
The first three segments which are segments one, two and three, are applied to the patient’s legs.
The fourth segment is applied to the pelvic area, while segments five and six are applied to the abdominal areas.
Segment five has a unique feature, a ball, which is applied directly on the umbilicus or the naval.
“When a patient experiences severe bleeding or shock, the body’s ability to maintain normal blood pressure and deliver oxygen to vital organs can be compromised”
Carren Siele
This enables it to apply compression on the uterus, reducing its size and hence allowing the abdominal segments to compress the blood vessels that are supplying the uterus.
The device ensures less blood is supplied to the uterus where it is less needed and to the vital organs that will eventually enable the patient to survive during obstetric haemorrhage
How does NASG work?
Carren Siele, a nursing officer in charge at Lwala Hospital narrates to us how the garment has been a game changer in maternal healthcare.
She explains that the garment works by applying external pressure to the lower part of the body, from the hips down to the feet.
The NASG is a simple but effective device that we have used to help to stabilize our patients in cases of severe bleeding or shock, and improve their chances of survival while they receive definitive care
Caren Siele
This pressure helps to push blood back up towards the heart and vital organs, which can become compromised in cases of severe bleeding or shock.
“When a patient experiences severe bleeding or shock, the body’s ability to maintain normal blood pressure and deliver oxygen to vital organs can be compromised,” said Carren.
“This can lead to organ failure, permanent injury, or even death.”
To prevent these complications, Carren says NASG is used to increase blood flow and maintain blood pressure until the underlying cause of shock can be addressed.
“The NASG is a simple but effective device that we have used to help to stabilize our patients in cases of severe bleeding or shock, and improve their chances of survival while they receive definitive care,” says Carren.
Which conditions do they use it?
However, she says that the garment is not to be used at all times during every delivery unless there is a justifiable need.
According to Carren, it is mostly used where hypovolemic shock (a condition caused by significant loss of blood or fluids from the body) occurs.
In such a situation, the resulting outcome is a drop in blood pressure and reduced oxygen delivery to vital organs.
The garment is then used for blood pressure until the underlying cause of shock can be addressed.
It can also be used in other conditions such as trauma or gastrointestinal bleeding, which are the main cause’s hypovolemic shock.
At what point does the doctor recommend its use
Carren outlines that the decision to use the device is solely reliant on the clinical assessment and judgment by the health provider.
“Before we decide to use the device on a patient, we consider factors such as the patient’s blood pressure, heart rate and other vital signs as well as the severity of bleeding,” she explained.




However, she warns that it is important to note that NASG is not a substitute for definitive treatment of the underlying cause of shock.
But, it is a temporary measure to stabilize the patient during transport while awaiting definitive care.
Pre NASG innovation
Before the innovation, healthcare providers like Carren were using traditional methods such as uterine massage and uterotonics (medication for stimulating uterine contraction) to manage PPH.
However, these methods were often inadequate, leading to a high mortality rate among women with PPH.
Since the invention of the NASG at the facility, Carren says their work especially in handling obstetric haemorrhage has been easy.
From the onset of this year, they have managed six patients in similar conditions by using the NASG garment.
“Through our organisation’s partnerships with the national government, we are working to ensure the NASG garment is listed as a life-saving commodity and have its taxes reduced”
Meshack Wafula
This has been aided by the Obstetric Haemorrhage Initiative (OHI).
OHI is a bundle of protocols and tools that treat obstetric haemorrhage cases.
It relies on lifesaving supplies like uterotonics, tranexamic acid and the uterine balloon tamponade and the NASG garment.
However, they require trained healthcare providers to know which tools to deploy and when.
Meshack Wafula, the coordinator of OHI training at Lwala Hospital says that they have expanded access to OHI across Migori County health facilities.

The Initiative tools
According to Meshack, they incorporate the use of tranexamic acid, uterine balloon tamponade (UBT), NASG and uterotonics to contain patients.
Tranexamic acid is a medication that works by reducing the breakdown of blood clots in the body.
“We commonly use the tranexamic acid in cases of heavy bleeding to help stop bleeding and promote clot formation,” said Meshack.
“It works by binding to the protein that dissolves blood clots, preventing it from breaking down the clots and allowing them to remain in place.”
On the other hand uterine balloon tamponade (UBT), is a medical procedure that involves placing a balloon inflated with fluid in the uterus.
The balloon puts pressure on the walls of the uterus and helps to stop the bleeding.
Similarly, Uterotonics are part medications that are administered through injection to stimulate the muscle cells in the uterus to shrink hence preventing excessive bleeding.
The OHI training program
Through the OHI training program, 322 healthcare providers have been trained as Trainer of Trainees (Tots) on the implementation of the OHI tools including the NASG.
Tots are cascaded down to mentor other healthcare workers from 214 primary health facilities across the county.
This targets a total of 3307 healthcare workers in the county.

All 214 facilities have been supplied with two NASG garments for dispensaries and up to eight garments for referral hospitals.
Lwala Community Alliance which is the innovator of NASG, has three garments for rotational use.
“Through our organisation’s partnerships with the national government, we are working to ensure the NASG garment is listed as a life-saving commodity and have its taxes reduced,” said Meshack.
“This will enable us to provide more pieces and also encourage counties access and purchase”
Changed narrative
So far, a total of 498 garments have been distributed across hospitals in Migori County, 72 in Homa Bay and 60 in Kilifi Counties.
Although NASG garment is not available locally. It is being imported and taxed as regular cloth with each garment going for Sh20, 000.
“I thought she had an accident or was cut by something. Unfortunately, she was bleeding after having childbirth
Beatrice Aketch
Beatrice Aketch is a midwife at Godkwer Dispensary.
She has been trained on how to use NASG.
“One day, I was working in our rural health dispensary when a couple came in. The woman had her leso soaked in blood in her clothes,” narrates Beatrice.
“I thought she had an accident or was cut by something. Unfortunately, she was bleeding after having childbirth.”
According to Beatrice, the patient had delivered her baby at home and when the bleeding won’t stop, her husband rushed her to the dispensary.
The community around Beatrice are a strong follower of LegioMaria church doctrines which prohibits hospital deliveries.
She says it is distressing to see mothers suffer during childbirth because of their religious beliefs.
“The woman was losing a lot of blood, and her blood pressure was dropping rapidly. I immediately knew that I had to take action to save her life,” added Beatrice.
“At that point, I decided to use the NASG as a part of the treatment protocol.”
She instructed her team to get the NASG and start wrapping it around the woman’s legs and pelvis.
They made sure that the device was snug but not too tight, so as not to impede blood flow.
Eventually, the woman’s vital signs observed showed her blood pressure was stabilizing, and the bleeding had decreased.
The NASG helped them buy time to get the woman to a county referral hospital for further treatment.

Reduced maternal mortality rates
Susan Agunda is a Trainer of Trainers and an NASG implementation program office at the Ministry of Health in Suna West Sub County.
Working as a supervisor overseeing the implementation of the garment at the sub-county level, she acknowledges the reduction in maternal deaths as compared to before.
In some facilities, you find that the garment is locked far from the delivery room. This poses a challenge to new staff who does not know where it is accessed
Susan Agunda
However, she outlined that the lack of readiness in most facilities has posed a bit of a challenge in the use of the garment.
“In some facilities, you find that the garment is locked far from the delivery room. This poses a challenge to new staff who does not know where it is accessed,” she outlined.
The innovation has seen a 38% reduction in mortality rate among women with PPH conditions across the county.

This is according to the 2022 Maternal and Perinatal Death Surveillance and Response (MPDSR) report.
Further NASG study conducted in 104 facilities in Migori reveals case fatality rate decreases from 2.60-1.32 %, indicating a 49% reduction.
There has been a tremendous reduction in blood transfusion services by 40.6% due to MASG use and a 20% reduction in clinical emergency hysterectomy.
Additionally, preliminary data from a study by the University of California San Francisco found a 70% decrease in maternal mortality.
This amounts to a 0.9 case fatality rate when the Obstetric Haemorrhage Initiative was operational.
The revelation shows a drastic reduction from a rate of 3.16 before the OHI program, a statistically significant improvement.
Of 2940 obstetrics haemorrhage cases recorded, 1051 NASG garments were used in the management of the cases.
Lwala has been instrumental in the implementation of NASGs in Migori to help reduce maternal deaths arising from PPH.
Lwala Community Alliance
Lwala Community Alliance is a non-profit organisation that works to improve the health, education and well-being of communities in rural western Kenya.
The organization operates a health centre at Lwala that provides comprehensive primary healthcare services.
Doreen Awino is the director of health systems at Lwala Community Alliance.
She highlights how poor communal healthcare and inaccessibility to better health facilities, lead the community of Lwala to donate land that gave birth to Lwala Community Alliance.
The main aim was to ensure that every person in the Lwala community could access health care.
However, when Migori County was listed among the top counties with high maternal mortalities, they took the initiative to bring a long-lasting solution.
This brought the NASG into action not only in Migori but also in Homa Bay and Kilifi counties.
“Lwala led the first county-wide scale-up of the NASG in Migori, and we were selected as the Kenyan government’s national training partner,” she noted.
Challenges in implementation
Despite the success and improved maternal healthcare in the community, the implementation and the use of NASG still face hurdles.
Although the garment provides a long period of use, 144 times, its poor management has rendered some useless.
The supportive staff has no knowledge of cleaning and storing the garment hence encouraging tear and wear.
Staff attrition is also another challenge derailing the success of this innovation.
This happens when a fully trained health provider resigns, retires or gets their contract terminated.
The evidence slows the progress and the uptake of innovation in various local health facilities. At times it also lowers the morale of other staff.

Poor referral services to a high-level hospital have been a big threat to saving the lives of patients.
This is heavily contributed to by poor road networks and the inaccessibility of facilities in remote areas, especially during the rainy season.
The lack of enough ambulances to ferry patients has also been a challenge, mostly when there is more than one case in one hospital.
The future of NASGs
NASGs are a simple yet effective solution for treating shock in obstetric patients, particularly those experiencing PPH.
Their low cost and ease of use make them an ideal solution for use in developing countries where access to more advanced medical technologies may be limited.
In addition to Lwala, other organizations such as the World Health Organization (WHO) and UNICEF have recognized the potential of NASGs.
The outcome has been the inclusion of their recommendations for the management of PPH, as their support will see the continued use of NASGs save countless lives around the world.
Lwala in collaboration with the government, developed the revised Emergency Obstetric Care (EMOC) Training and Mentorship Guide, which now includes OHI.
With this in place, counties can adopt the use of OHI protocols and interventions.
Lwala is also partnering with the government in OHI training and is working closely with Kenya Medical Training Colleges to include OHI in the nursing school curriculum.

[…] This article was first published in Lake Region Bulletin […]